Lab Insights Solutions
Routine Test Management
The first automated solution customized to individual plan requirements, ensuring effortless compliance with routine lab policies.
Industry Challenge:
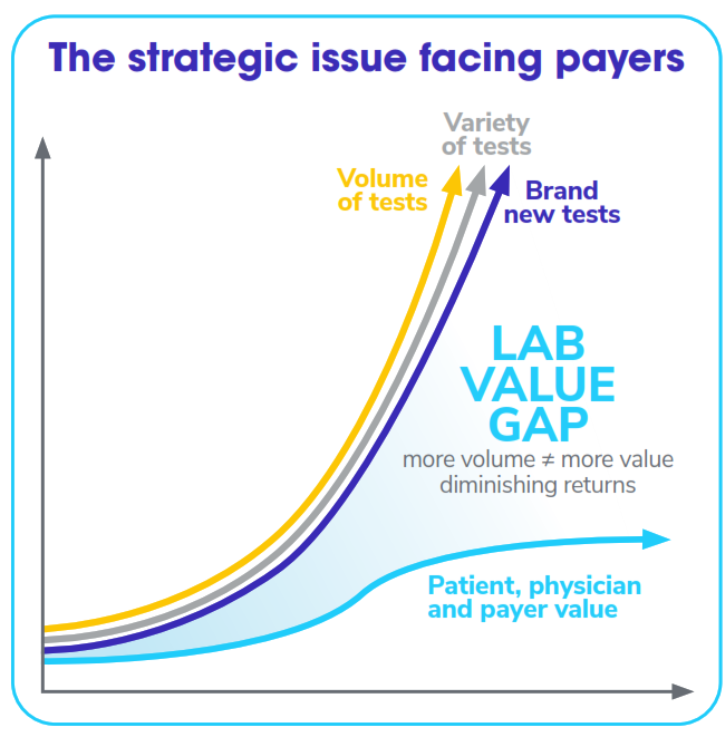
Consider how essential lab testing is to healthcare.
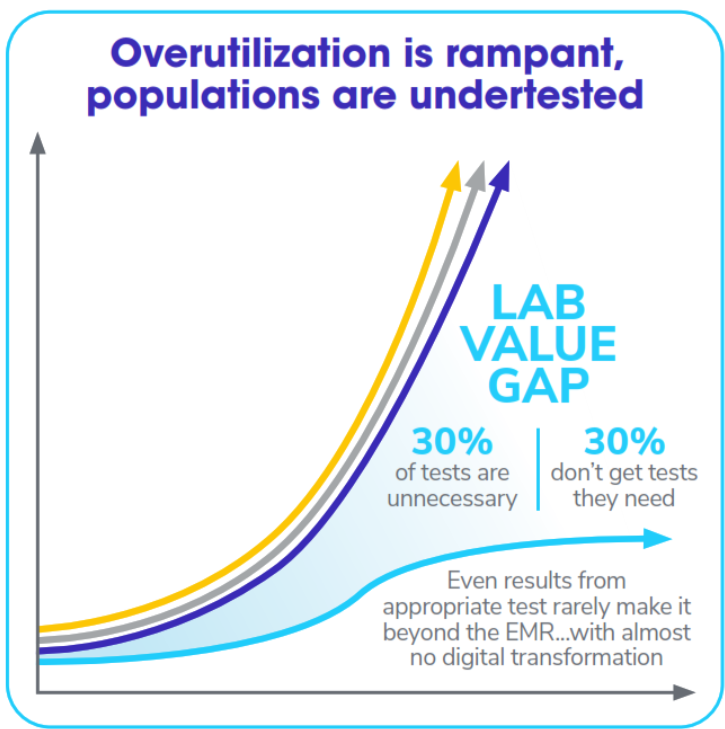
Around 14 billion clinical lab tests are performed annually in the U.S., making them the most utilized medical benefit. Lab results are involved in roughly 70% of clinical decisions. Despite their importance, around 30% of lab tests conducted in the U.S. may be unnecessary, while another 30% of patients don’t get the test they genuinely need.
And lab testing is expensive. In 2021, Medicare alone spent $9.3 billion on tests, a record 17% increase from the previous year.
Avalon’s Lab Insights Solutions work together to arm you with critical lab-driven insights to accelerate your value-driven care success.
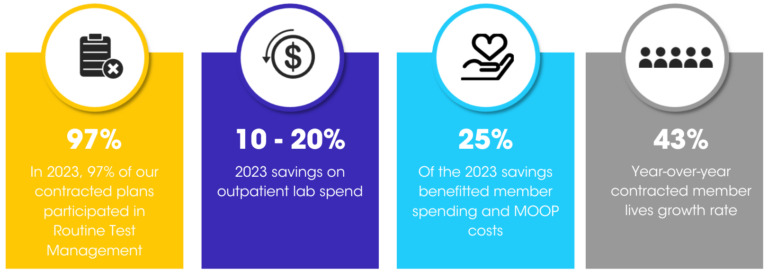
Avalon is the only company with an automated Routine Test Management solution to ensure lab testing follows clinical guidelines, resulting in savings ranging from $1 to $3 PMPM, and independent from plans’ payment integrity efforts.
Our Solution:
Our flagship solution, Avalon’s Routine Test Management (RTM), streamlines the process of determining coverage criteria to eliminate unnecessary utilization of high-volume, low-cost laboratory tests while ensuring that physicians and patients are unaffected.
10 – 20% savings on outpatient routine lab spend in 2023
Routine Test Management Overview:
Avalon has streamlined routine clinical lab test management with its Routine Test Management (RTM) solution. Not a replacement for payment integrity and claims editing solutions, the cloud-based RTM application is tailor-made to manage laboratory policies and enable health plans to experience unmatched precision and efficiency in claims processing.
Avalon’s RTM solution delivers decision advice codes that guide approving, reducing, or denying claim lines. The solution also includes references to specific policy details supporting the decision, ensuring transparency and fairness in claims processing.
Integrating the RTM solution with a payer’s adjudication system simplifies lab claim review against fixed criteria, thus ensuring compliance with laboratory policies. The automated solution is highly configurable and can apply various filters based on the line of business, provider, and place of service, making it a perfect fit for all routine test management needs.
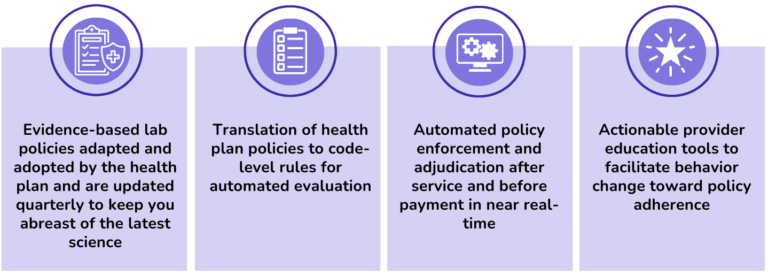
- Grounded in science: Avalon’s Lab Clinical Policies for outpatient lab tests are based on scientific research and undergo a rigorous review process. Our dedicated full-time scientists write and maintain all the policies in-house, including PhDs. Each policy has a solid scientific foundation, with an average of 50 references used to support it.
- Clinical Advisory Board: Policies are updated annually or as science dictates by an independent Clinical Advisory Board (CAB) consisting of industry leaders in laboratory medicine. To learn more about our CAB members, please visit www.avalonhcs.com/who-we-are
- Policy approval and translation: The established policies are translated into codified rules and edits to ensure compliance with the health plan’s standards. The health plan has full control over the adoption and approval of policies, with medical sign-off taking place at the policy level. Avalon oversees the configuration of rules, ensuring they align with the approved policies and comply with quality and compliance standards.
- Policy enforcement: Using the software, coverage criteria, and clinical policy compliance are made transparent. During mid-adjudication, automated decision-making information, including the reason for denial and the associated, approved clinical policy, is sent to the health plan within milliseconds for final determination.
- Provider education: Avalon’s implementation and ongoing support provide education and tools to help providers adhere to policy, bill appropriately, and reduce burden.
Our Values: